Empowering Healthcare Excellence Since 2015

Contact Us :

9960 NW 116th Way #13,
Medley, FL, USA 33178

What is the MACRA Quality Payment Program?
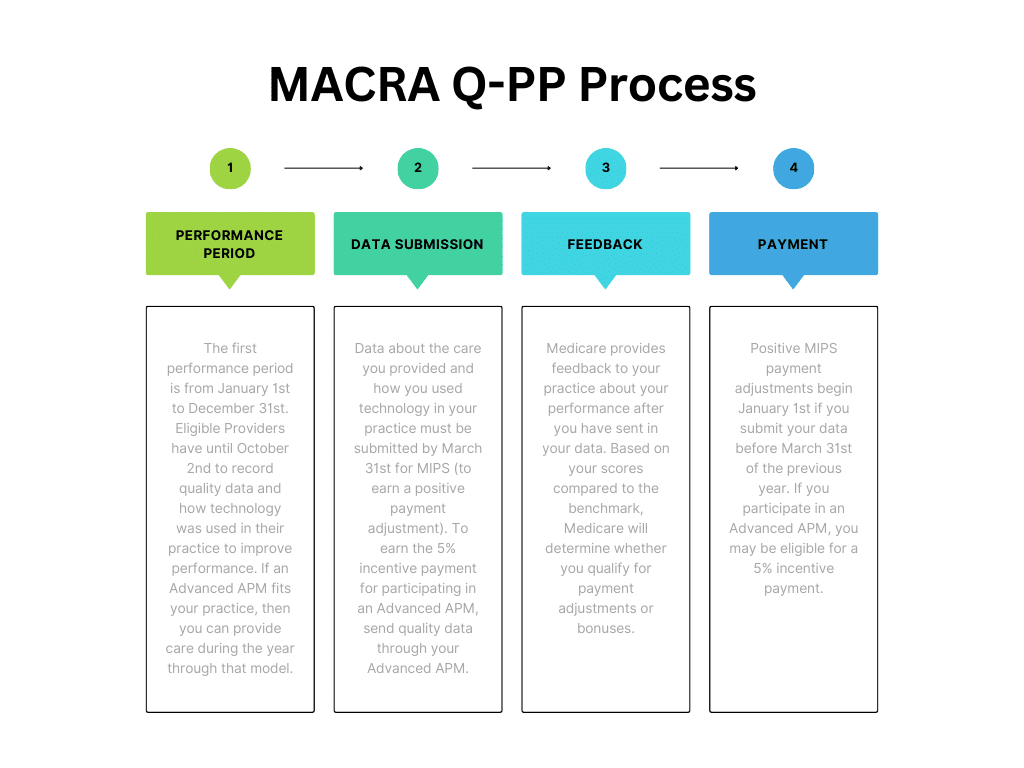
The Quality Payment Program improves Medicare by helping you focus on care quality and the one thing that matters most — making patients healthier. The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) ended the Sustainable Growth Rate formula, which threatened clinicians participating in Medicare with potential payment cliffs for 13 years. If you participate in Medicare Part B, you are part of the dedicated team of clinicians who serve more than 55 million of the country’s most vulnerable Americans, and the Quality Payment Program’s purpose is to provide new tools and resources to help you give your patients the best possible care. You can choose how you want to participate based on your practice size, specialty, location, or patient population. The Quality Payment Program has two tracks you can choose:
These payment models prioritize rewarding quality and efficiency over service volume. In APMs, physicians play a central role in coordinating comprehensive patient care, utilizing technology for informed decision-making. These models prioritize preventive measures and resource optimization to enhance outcomes while managing costs. Embracing APMs offers physicians incentives for delivering high-quality, cost-effective care.
If you decide to participate in an Advanced APM through Medicare Part B you may earn an incentive payment for participating in an innovative payment model.
A program under the Medicare Access and CHIP Reauthorization Act (MACRA) designed to incentivize healthcare providers to meet specific benchmark scoring requirements in order to improve care quality and performance. MIPS evaluates clinicians based on four performance categories: Quality, Cost, Promoting Interoperability, and Improvement Activities. Clinicians report data on these categories, and their performance determines payment adjustments. MIPS provides a framework for clinicians to enhance care quality, optimize costs, and engage in activities that support care improvement. Participation in MIPS offers incentives for clinicians to deliver high-quality, efficient care while meeting reporting requirements.
If you decide to participate in traditional Medicare Part B, then you will participate in MIPS where you can earn a performance-based payment adjustment.
Who is Eligible for Participation in the Quality Payment Program?
You’re a part of the Quality Payment Program if you bill Medicare more than $30,000 a year, provide care for more 100 Medicare patients a year, and are one of the following: